Features
- Non-invasive beat-to-beat hemodynamic parameters such as Cardiac Output and Stroke Volume
- Optimized for trending
- Absolute CO accuracy through calibration
Parameters
- Cardiac Output (CO & CI)
- Stroke Volume (SV & SVI)
- Systemic Vascular Resistance (SVR & SVRI)
- Cardiac contractility (dP / dt)
- Left Ventricular Ejection Time (LVET)
- Maximal surface of the aorta
- Rate pressure product (RPP)
- Model computation of the aortic flow waveform (mFlow)
- Systolic pressure time index (SPTI)
- Diastolic pressure time index (DPTI)
- DPTI/SPTI ratio
- Aortic Impedance (Zao)
- Windkessel Compliance (Cwk)
- Peripheral Resistance (Rp)
- Baroreceptor Sensitivity (BRS)
Advanced Hemodynamics
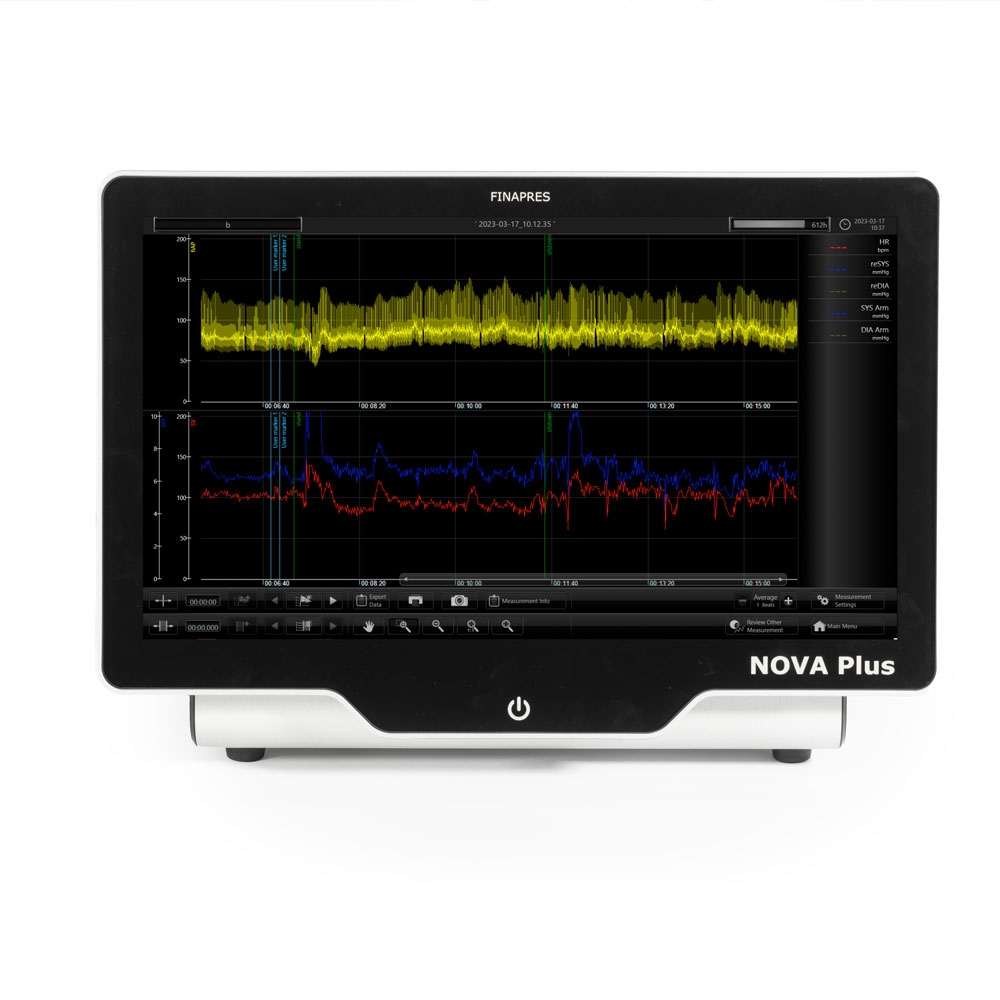
As an example of a potential application of the HD software, the image shows the immediate blood pressure (reBAP), heart rate, CO and SV response during a stand test recorded with the Finapres® NOVA.
First plot: reBAP signal. Second plot: CO and SV. Third plot: RR interval (requires ECG+resp configuration)
References
- Wesseling, K. H., et al. “Computation of aortic flow from pressure in humans using a nonlinear, three-element model.” Journal of applied physiology 74.5 (1993): 2566-2573.
- Harms, Mark PM, et al. “Continuous stroke volume monitoring by modelling flow from non-invasive measurement of arterial pressure in humans under orthostatic stress.” Clinical Science 97.3 (1999): 291-301.
- Jansen, J. R. C., et al. “A comparison of cardiac output derived from the arterial pressure wave against thermodilution in cardiac surgery patients.” British journal of anaesthesia 87.2 (2001): 212-222.
- Leonetti, Pascal, et al. “Stroke volume monitored by modeling flow from finger arterial pressure waves mirrors blood volume withdrawn by phlebotomy.” Clinical Autonomic Research 14.3 (2004): 176-181.
- Bogert, Lysander WJ, and Johannes J. van Lieshout. “Non‐invasive pulsatile arterial pressure and stroke volume changes from the human finger.” Experimental physiology 90.4 (2005): 437-446.

.jpg)




